How to Talk To Your Pediatrician About Your Child’s Weight
Measuring a child’s height and weight is a typical part of any well-child visit or annual check-up. It’s an important tool for measuring your child’s growth and development. But weight is also just one part of the equation when it comes to a child’s health.
What’s more, it can be a challenging topic to address with kids, who, according to some data, may form opinions about their body image as young as age 3.
In this post, we’ll dive into why a child is weighed by the pediatrician in the first place, what weight can - and can’t - tell us about a child’s health, and how to navigate these discussions with your child and your pediatrician.
Why do we measure children’s weight?
While one weight measurement at one point in time doesn’t tell us much about a child’s health, tracking a child’s weight over time is a useful tool. A child’s weight trajectory is a key metric for assessing healthy growth and development.
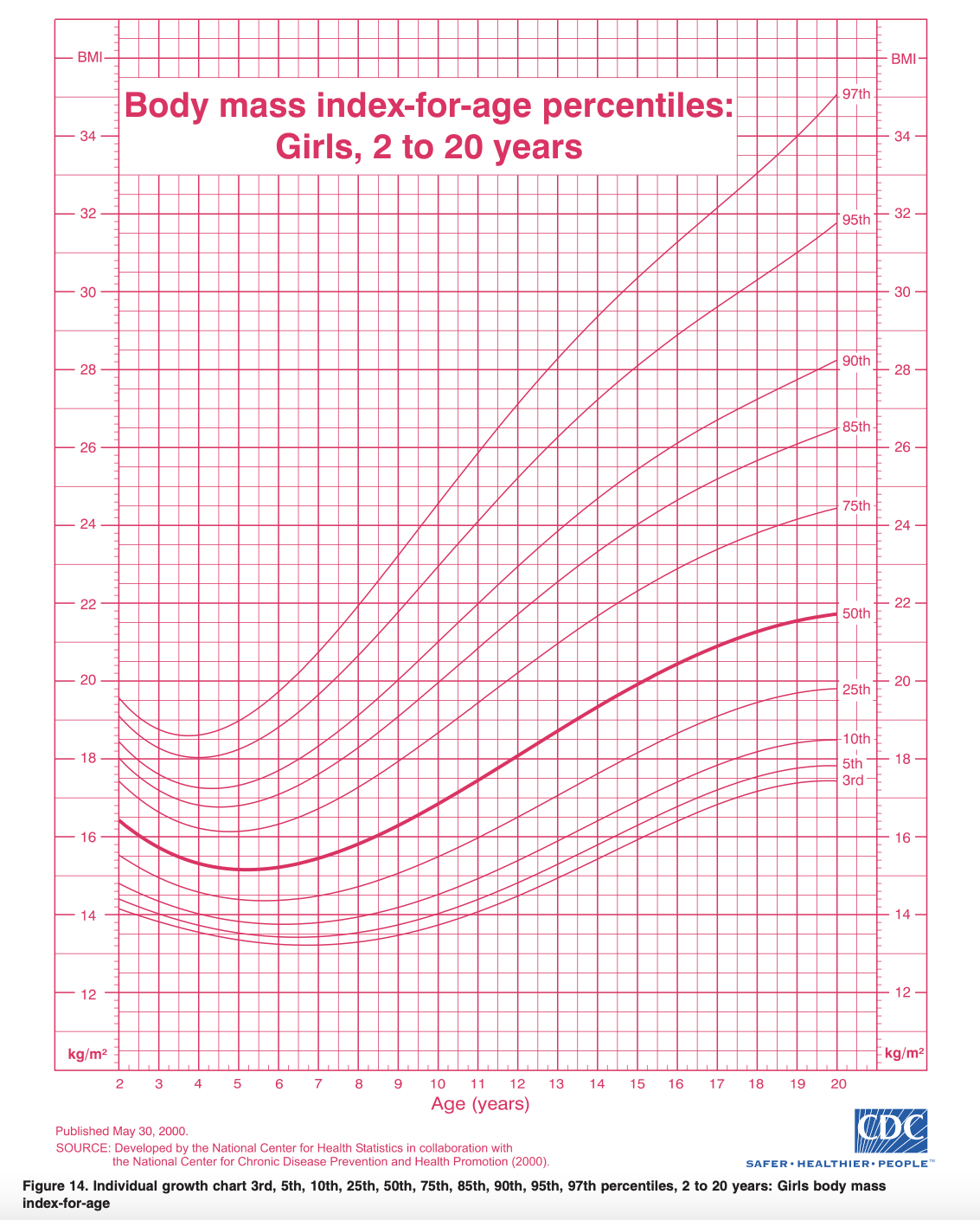
Typically, a child’s weight and height are assessed using the CDC’s pediatric growth charts. These charts allow us to compare a child’s height, weight, and body mass index (BMI) to other children of the same age and gender. For children under 24 months old, separate charts are used to track weight-for-length, weight-for-age, length-for-age, and head circumference (a marker of how baby’s brain is growing).
On both types of charts, you’ll find height (or length for children under 24 months) and weight along the left and right sides, and age at the top and bottom. The curved lines are percentile numbers that tell us where, within a large sample, your child’s height/length and weight fall compared to other children of the same age and gender. For example, if your child is in the 40th percentile for height, that means they are taller than 40% of children of the same age and gender. What’s important to pay attention to is not the percentile itself, but rather whether your child is tracking along the same curve as they get older.
What weight can tell us about a child’s health
Say your child has consistently been tracking at around the 50th percentile for weight, but at their next well visit, they’re now at the 25th percentile for weight. This change in growth trajectory would alert your pediatrician to explore what has caused the significant dip in percentiles. They might ask if your child has had changes in appetite, stress levels, activity levels, or bowel habits, for example.
If your child is experiencing a delay in weight gain or even weight loss, your pediatrician can then determine appropriate interventions to help ensure that your child is getting the nutrients they need to grow and thrive.
The same goes for a situation in which a child was tracking along the 50th percentile for weight and then suddenly jumps up to the 70th percentile.
Maybe the child has just gone through a growth spurt, become more sedentary, or started taking medication that leads to weight gain. Perhaps something else has changed that requires an intervention. Either way, tracking the changes in percentiles over time helps healthcare providers determine whether appropriate interventions are needed to help a child get back on track.
What weight can’t tell us about a child’s health
While measuring weight and using pediatric growth charts is one part of the overall picture, they’re just one of many tools we can rely on to help measure a child’s health.
For babies and toddlers, reaching developmental milestones, such as learning to wave, smile, or crawl, are important markers of growth and health.
And for children of all ages, larger trends like the child’s appetite, bowel habits, and levels of physical activity over time can tell us much more about their health than a number on the scale.
It’s also important to note that a child can be healthy at any percentile, whether they’re at the fifth or ninety-fifth percentile for height or weight; what really matters is the overall velocity of growth and significant dips or spikes in growth along the way.
Discussing weight with children
Weight is important to track to assess children’s growth and development. Kids who aren’t keeping up with their growth trajectories may be at risk for failure to thrive, as well as other health problems which can cause delays in physical and motor skills, as well as social and cognitive learning.
On the other hand, children with overweight and obesity have an increased risk for heart disease, diabetes, high blood pressure, and other chronic diseases later in life.
The American Academy of Pediatrics (AAP), which recently published new guidelines on managing overweight and obesity in children and adolescents, currently recommends that treatment for these conditions start as early as possible. The guidelines have come under fire for their aggressive approach, which recommends weight-loss drugs for kids with obesity as young as 12 and bariatric surgery for kids with severe obesity as young as 13.
As a pediatric dietitian specializing in child nutrition with over 13 years of experience, I agree with the many registered dietitians and eating disorder specialists who are concerned that the guidelines’ increased focus on BMI and weight, rather than overall health and well-being, is misguided – and potentially damaging to children’s mental and physical health.
Research shows that kids experience the negative impacts of weight talk at increasingly younger ages. Remember: all children are growing and therefore need to gain weight to support continued growth. But young children are concrete thinkers, so when they hear weight gain as something to avoid – whether from TV, social media, or the adults around them – they equate weight gain to “bad.” In fact, a recent study showed that children as young as 6 years old may experience disordered eating behaviors. These behaviors, in turn, can lead to an eating disorder, anxiety, and/or depression in children and teens.
Weight talk also encourages dieting, which has several risks for children and teens. It disrupts a child’s ability to recognize their inner hunger and fullness cues, which can lead to weight cycling and yo-yo dieting. Restrictive diets can also prevent kids from adopting healthy eating habits and getting the wide variety of macro- and micronutrients they need to grow and develop.
So how do we model healthy habits without negatively impacting a child’s relationship with food and their body?
Most importantly, focus on and role model healthy lifestyle behaviors - such as getting enough sleep, including a wide variety of foods to provide fuel and energy, and finding fun ways to get physical activity - rather than weight. Eating family meals together, getting kids involved with preparing and cooking food, and focusing on mindful eating are also great ways to foster healthy habits that have nothing to do with weight. If you have a weight scale in your home, consider putting it away or getting rid of it, so your child doesn’t become focused on their weight and how it changes as they grow. (For more tips on discussing weight, body image, and health with kids, check out my post on how to talk to kids about weight).
How to talk to your pediatrician about your child’s weight?
The bottom line? We can still weigh children and benefit from the information we glean from tracking weight velocity, while also protecting our children from weight talk. That’s why I recommend that children not be part of conversations about weight.
So, at the pediatrician’s office or with the school nurse, be polite but firm and make it clear that any discussion of your child’s weight should not occur in front of your child. If your pediatrician or other healthcare provider has concerns about your child’s weight, let them know you’re happy to discuss it without your child present.
If you’re struggling with the idea of talking to your pediatrician about not discussing weight with your child present, I’ve put together some language that might be useful. Try writing the following on a card and handing it to the doctor or nurse at the start of the appointment:
“I’d prefer that any discussion about [your child’s name]’s weight be from one adult to another, so please don’t discuss weight in front of [your child’s name].”
Most pediatricians will be more than happy to accommodate this request!
Overall, remember that the number on the scale is just that - a number. Remind your child that all bodies are good bodies and that bodies come in all shapes and sizes, and continue to encourage behaviors that are healthy for the body, mind, and soul. And remind yourself that you’re doing a great job as a parent, too!
Have you tried having this discussion with your pediatrician or other healthcare provider, and if so, what’s worked well? Please share in the comments below…
And if you're concerned about your child’s growth, appetite, or weight, I am currently accepting new clients in my virtual private practice - book a session at your convenience and we will explore personalized solutions and ways to navigate your concerns together.
Big thanks to dietetic intern, Eva Lewandowski for her contributions to this blog post!